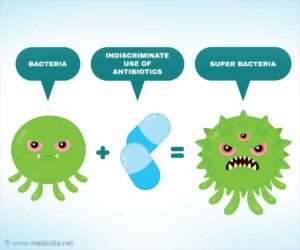
Antibiotics are drugs that treat or prevent bacterial infections. Antibiotic resistance occurs when bacteria develop the ability to withstand antibiotics that were designed to kill or prevent them from growing.
Bacteria become antibiotic resistant such that even when exposed to antibiotics, these antibiotic-resistant bacteria can thrive, multiply, and infect the host. These bacteria have the ability to infect both humans and animals, and the diseases they cause are no longer treatable with certain antibiotics.
This has a significant impact on our ability to prevent and treat chronic diseases, increasing recovery times, hospital stays, and death rates.
Facts:
- In 2019, antimicrobial resistance killed at least 1.27 million people and caused nearly 5 million deaths, making it a major global public health concern.
- In Nigeria, about 42% of adults and 47% – 71% of children use antibiotics indiscriminately without prescription.
- In the United States, more than 2.8 million antimicrobial-resistant infections occur each year.
- More than 35,000 people die as a result of antibiotics resistance, according to the CDC’s 2019 figures.
- Antimicrobial resistance can affect people of all ages, and any country.
- It affects almost all industries, not sparing the healthcare, veterinary, and agricultural industries.
- As a result, it is one of the most pressing public health issues in the world.

Causes of Antibiotics Resistance:
Generally. antimicrobial resistance develops naturally, but it is aided by;
- inappropriate medication use, such as using antibiotics for viral infections such as the common cold or flu, or sharing antibiotics.
- failing to finish an antibiotic as prescribed. If you stop taking it too soon, you may not be able to eliminate all of the bacteria. The bacteria that remain may develop resistance.
- medications of poor quality.
- prescription errors.
- unsanitary and unhygienic conditions.
- insufficient infection prevention and control.
- inadequate food handling.
- administration of antibiotics to healthy animals in order to promote growth and prevent disease. Antibiotic-treated farm animals are more likely to develop drug-resistant bacteria, which can then spread to people who consume meat products. As a result, infections in humans caused by resistant bacterial strains are more difficult to treat.
Dangers of Antibiotics Resistance:
- Treatment failure and a more prolonged infection with recurrence.
- Increased risk of other illnesses.
- Longer stay in hospitals.
- Economic and financial strains.
- Decreased productivity in society.
- Increased death.

Prevention and Control:
Antibiotic prescribing and use must urgently change around the world. Even if new medications are developed, antibiotic resistance will remain a serious threat unless behavior changes.
The following measures should be adopted;
- Antibiotics should not be used to treat a virus.
- Don’t save an antibiotic for the next time you get sick.
- Antibiotics should be taken as directed. Do not skip any doses. Even if you are feeling better, complete the entire course of treatment.
- Never take an antibiotic that has been prescribed for someone else.
- To stop the spread of diseases, behavior changes must also focus on improving food hygiene, hand washing, practicing safer sex, and getting vaccinated.
- Medical professionals can also help by: only prescribing antibiotics when absolutely necessary; ensuring that the medication is directed at the specific bacteria at issue; and only prescribing medications for as long as absolutely necessary.
- The government should establish effective disease control surveillance and provide disease detection, treatment, and prevention tools.
Conclusion:
Antibiotics’ exceptional health benefits are jeopardized by the rapid emergence of resistant bacteria. This crisis is widespread due to the overuse of these medications around the world, as well as a lack of new antibiotic agents being developed by pharmaceutical companies to address the problem.
Antibiotic-resistant infections place a significant financial and health burden on healthcare systems. It is critical to collaborate in order to implement new regulations, increase research efforts, and develop crisis management strategies.